A team at the Hong Kong University of Science and Technology has decoded the genome of the volcano-dwelling scaly-foot snail, which can live in remarkably hot temperatures.



Stem Cell Neurotherapy, which has achieved successful results with Parkinson’s, Essential Tremor, and Brain Tumor, can generate new cells and tissues in the lungs, liver, kidney, etc., to replace those cells and tissues that have been infected by COVID-19. This will improve the lung microenvironment, protect lung alveoli epithelial cells, and restore healthy functioning lungs.
These new cells will eliminate the fever, coughing, headaches, breathing problems, and other symptoms related to COVID-19.
At the 9:03 minute mark on the Stem Cell Neurotherapy recording, you will hear the therapeutic message:
“Your stem cells are going to transform themselves into new lung, liver, kidney, and other cells to replace those cells that have been infected by the Coronavirus. This will eliminate the inflammation, fever, breathing difficulties, coughing, and other symptoms caused by the virus.
Your body is going to produce healing hormones, messenger molecules, and proteins which will transform the stem cells into mature, well-functioning connections and tissues. These new cells and tissues are going to replace those cells and tissues that have been infected by the virus.
Your stem cells are going to transform themselves into T-Cells, B-Cells, and Natural Killer Cells, which will seek out, identify, attack, and destroy all the Coronavirus cells in your entire body.”
face_with_colon_three could heal body parts in humans.
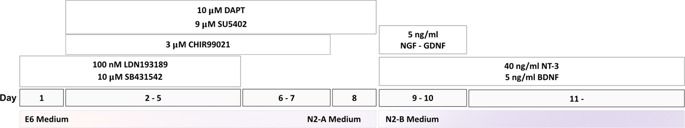
The generation of human induced pluripotent stem cells (iPSCs) from somatic cells using gene transfer opens new areas for precision medicine with personalized cell therapy and encourages the discovery of essential platforms for targeted drug development. iPSCs retain the genome of the donor, may regenerate indefinitely, and undergo differentiation into virtually any cell type of interest using a range of published protocols. There has been enormous interest among researchers regarding the application of iPSC technology to regenerative medicine and human disease modeling, in particular, modeling of neurologic diseases using patient-specific iPSCs. For instance, Parkinson’s disease, Alzheimer’s disease, and spinal cord injuries may be treated with iPSC therapy or replacement tissues obtained from iPSCs. In this review, we discuss the work so far on generation and characterization of iPSCs and focus on recent advances in the use of human iPSCs in clinical setting.
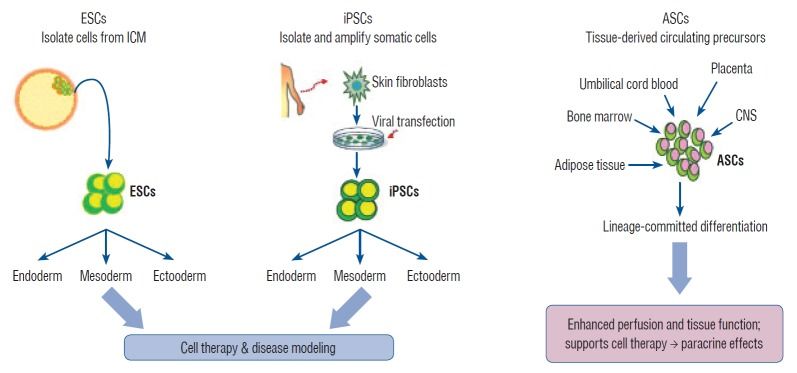
Stem cells exhibit the capacity of self-renewal and may undergo differentiation into various tissue types. These are divided into pluripotent stem cells (PSCs; embryonic stem cells [ESCs] and induced pluripotent stem cells [iPSCs]) and multipotent stem cells (adult stem cells [ASCs]) based on their differentiation capacity [45]. PSCs, including ESCs derived from embryos and iPSCs derived by gene transfer, may undergo indefinite proliferation and differentiate into different types of tissues depending on the treatment conditions [86]. Multipotent stem cells, however, may be obtained from tissue-derived precursors (umbilical cord blood, bone marrow, adipose tissue, placenta, or blood), which are already grown tissues.

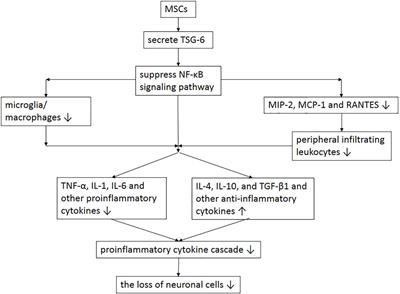
Traumatic brain injury (TBI) is an important cause of human mortality and morbidity, which can induce serious neurological damage. At present, clinical treatments for neurological dysfunction after TBI include hyperbaric oxygen, brain stimulation and behavioral therapy, but the therapeutic effect is not satisfactory. Recent studies have found that exogenous stem cells can migrate to damaged brain tissue, then participate in the repair of damaged brain tissue by further differentiation to replace damaged cells, while releasing anti-inflammatory factors and growth factors, thereby significantly improving neurological function. This article will mainly review the effects, deficiencies and related mechanisms of different types of stem cells in TBI.
Traumatic brain injury (TBI) is a common and frequently occurring disease. According to the World Health Organization, TBI will become the main cause of human mortality and morbidity after 2020, which brings a heavy economic burden to patients and families (Maas et al., 2017). TBI is a disease which causes the destruction of normal brain function, and leads to serious physical, cognitive and emotional disorders. The pathophysiology of TBI mainly includes the break of the blood brain barrier (BBB), extensive neuroinflammation, diffuse axonal injury, and neurodegenerative lesions (Xiong et al., 2008). The pathological changes of brain injury are mainly the loss of normal tissue structure, destruction of neuronal cells and internal environment disturbance, among which neuronal cells injury is the key point. There is no effective drug treatment so far.
Inducing human pluripotent cells.
Scientific Reports volume 10, Article number: 7752 (2020) Cite this article.
A woman walking down the street hears a bang. Several moments later she discovers her boyfriend, who had been walking ahead of her, has been shot. A month later, the woman checks into the emergency room. The noises made by garbage trucks, she says, are causing panic attacks. Her brain had formed a deep, lasting connection between loud sounds and the devastating sight she witnessed.
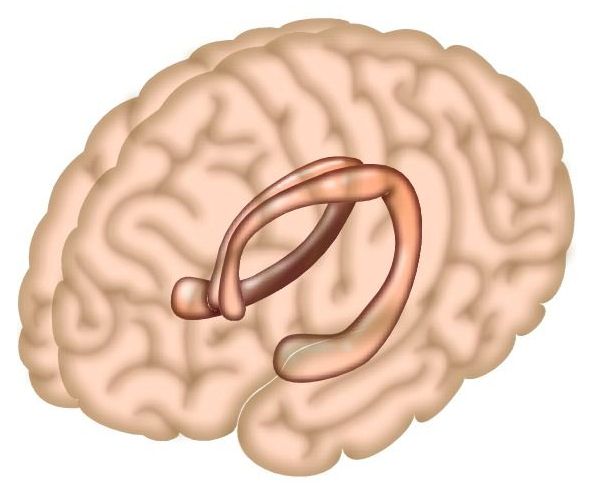
This story, relayed by clinical psychiatrist and co-author of a new study Mohsin Ahmed, MD, Ph.D., is a powerful example of the brain’s powerful ability to remember and connect events separated in time. And now, in that new study in mice published today in Neuron, scientists at Columbia’s Zuckerman Institute have shed light on how the brain can form such enduring links.
The scientists uncovered a surprising mechanism by which the hippocampus, a brain region critical for memory, builds bridges across time: by firing off bursts of activity that seem random, but in fact make up a complex pattern that, over time, help the brain learn associations. By revealing the underlying circuitry behind associative learning, the findings lay the foundation for a better understanding of anxiety and trauma- and stressor-related disorders, such as panic and post-traumatic stress disorders, in which a seemingly neutral event can elicit a negative response.
A state-of-the-art disinfectant developed by the Israel Institute for Biological Research and distributed by Tera Novel is capable of killing 100% of bacteria, viruses, molds and some fungi, including the novel coronavirus.
“Our disinfectant works in a very different way from many others,” Tera Novel chairwoman Karen Cohen Khazon told The Jerusalem Post. “We also use hypochlorite, but in a very high [concentration] and we add some [additional ingredients] so that anywhere the disinfectant is sprayed, it becomes a very white film of gel which keeps the [material] on the surface for a while.”
Scientists have successfully developed a new technique to reliably grow crystals of organic soluble molecules from nanoscale droplets, unlocking the potential of accelerated new drug development.
Chemistry experts from Newcastle and Durham universities, working in collaboration with SPT Labtech, have grown the small crystals from nanoscale encapsulated droplets. Their innovative method, involving the use of inert oils to control evaporative solvent loss, has the potential to enhance the drug development pipeline.
Whilst crystallization of organic soluble molecules is a technique used by scientists all over the world, the ability to do so with such small quantities of analyte is ground-breaking.
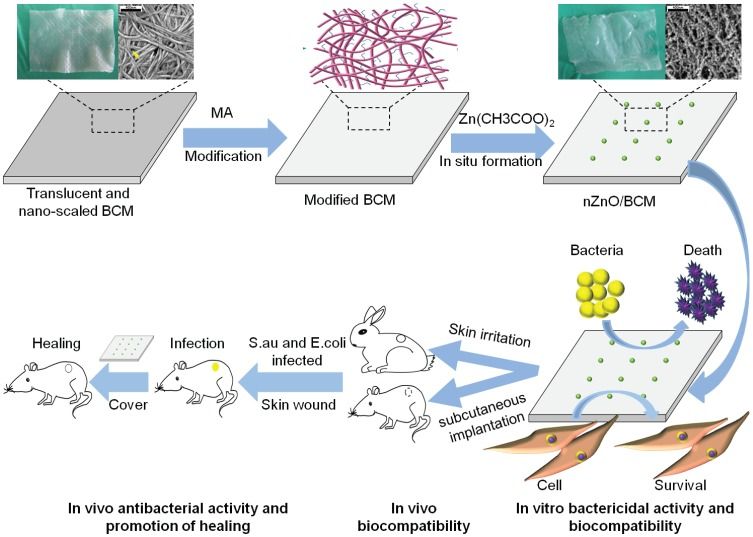
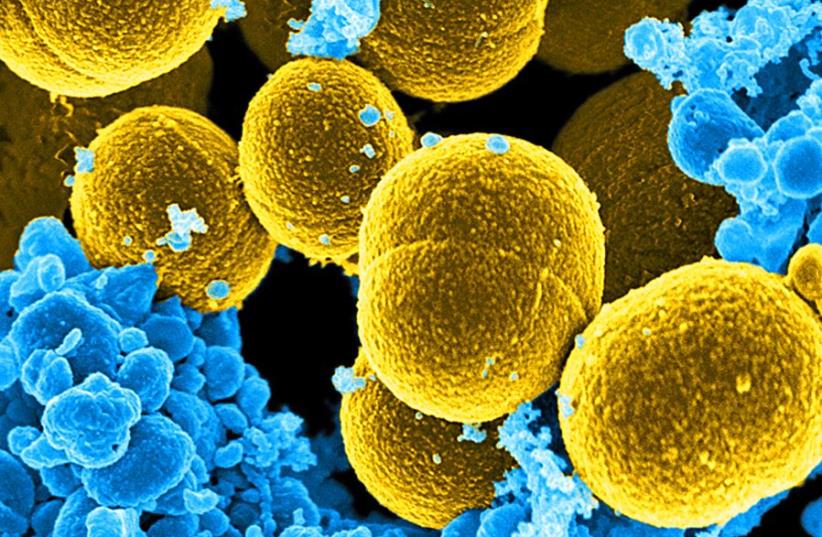
Developing an ideal wound dressing that meets the multiple demands of safe and practical, good biocompatibility, superior mechanical property and excellent antibacterial activity is highly desirable for wound healing. Bacterial cellulose (BC) is one of such promising class of biopolymers since it can control wound exudates and can provide moist environment to a wound resulting in better wound healing. However, the lack of antibacterial activity has limited its application.
We prepared a flexible dressing based on a bacterial cellulose membrane and then modified it by chemical crosslinking to prepare in situ synthesis of nZnO/BCM via a facile and eco-friendly approach. Scanning electron microscopy (SEM) results indicated that nZnO/BCM membranes were characterized by an ideal porous structure (pore size: 30~ 90 μm), forming a unique string-beaded morphology. The average water vapor transmission of nZnO/BCM was 2856.60 g/m2/day, which improved the moist environment of nZnO/BCM. ATR-FITR further confirmed the stepwise deposition of nano-zinc oxide. Tensile testing indicated that our nanocomposites were flexible, comfortable and resilient. Bacterial suspension assay and plate counting methods demonstrated that 5wt. % nZnO/BCM possessed excellent antibacterial activity against S.aureus and E. coli, while MTT assay demonstrated that they had no measurable cytotoxicity toward mammalian cells.