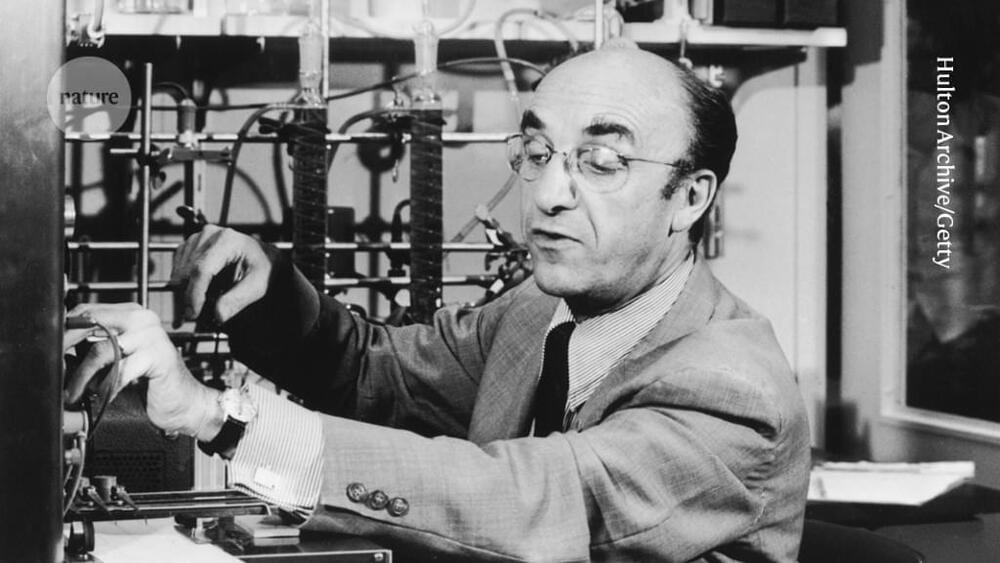
Roger Guillemin identified the molecules in the brain that control the production of hormones in endocrine glands such as the pituitary and thyroid. His work led to a torrent of advances in neuroendocrinology, with far-reaching effects on studies of metabolism, reproduction and growth. For his discoveries on peptide-hormone production in the brain, Guillemin shared the 1977 Nobel Prize in Physiology or Medicine with Andrew Schally and Rosalyn Yalow. He has died at the age of 100.
In the autumn of 1969, after analysing millions of sheep brains for more than a decade, Guillemin and his colleagues determined the structure of thyrotropin-releasing factor (TRF). This small peptide is produced in the hypothalamus, a small region at the base of the brain, and is transported to the anterior lobe of the nearby pituitary gland, where it triggers the release of the hormone thyrotropin. Thyrotropin, in turn, stimulates the thyroid gland to produce the hormone thyroxine, which regulates metabolic activity in nearly every tissue of the body. More than two dozen drugs use such hypothalamic hormones to treat endocrine disorders and cancers, and the worldwide market for these drugs is worth several billion dollars.
Guillemin was born in Dijon, France, and came of age at the end of the Second World War. He graduated from medical school in the University of Lyon, France, in 1949 and worked as a country doctor in the small commune of Saint-Seine-l’Abbaye in Burgundy. He found the work satisfying but intellectually limiting, noting that “in those days I could take care of all my patients with three prescriptions, including aspirin”. Fascinated by how the brain and pituitary gland control the body’s response to stress, he attended lectures in Paris by the Hungarian–Canadian endocrinologist Hans Selye, after which Selye accepted Guillemin’s request to spend a year doing research in his laboratory at the University of Montreal, Canada.