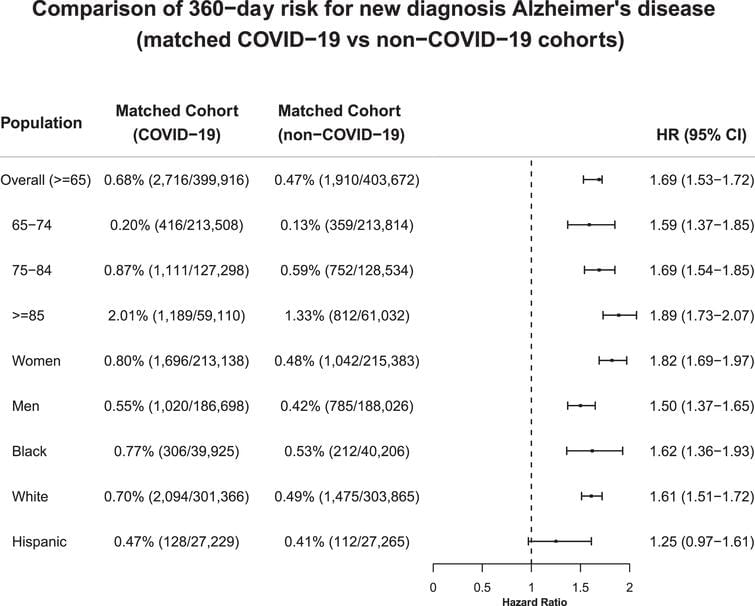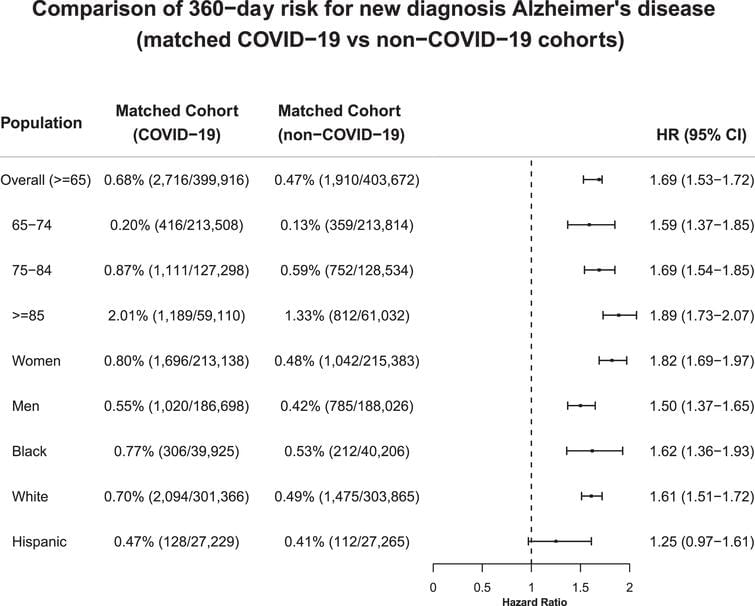
The study population comprised 6,245,282 older adults (age ≥65 years) who had medical encounters with healthcare organizations between 2/2/2020–5/30/2021 and had no prior diagnosis of Alzheimer’s disease. The population was divided into two cohorts: 1) COVID-19 cohort (n = 410,748)— contracted COVID-19 between 2/2/2020–5/30/2021; 2) non-COVID-19 cohort (n = 5,834,534)— had no documented COVID-19 but had medical encounters with healthcare organizations between 2/2/2020–5/30/2021. The status of Alzheimer’s disease and COVID-19 were based on the International Classification of Diseases (ICD-10) diagnosis codes and laboratory tests (details in the Supplementary Material).
We examined risks for new diagnosis of Alzheimer’s disease in COVID-19 and non-COVID-19 cohorts in all older adults, three age groups (65–74, 75–84, ≥85), and three racial/ethnic groups (Black, White, and Hispanic). Cohorts were propensity-score matched (1:1 using a nearest neighbor greedy matching) for demographics, adverse socioeconomical determinants of health including problems with education, occupational exposure, physical, social and psychosocial environment, and known risk factors for Alzheimer’s disease [13] (details in the Supplementary Material). Kaplan-Meier analysis was used to estimate the probability of new diagnosis of Alzheimer’s disease within 360 days after the COVID-19 diagnosis. Cox’s proportional hazards model was used to compare matched cohorts using hazard ratios and 95% confidence intervals. All statistical tests were conducted within the TriNetX Advanced Analytics Platform at significance set at p < 0.05 (2-sided).