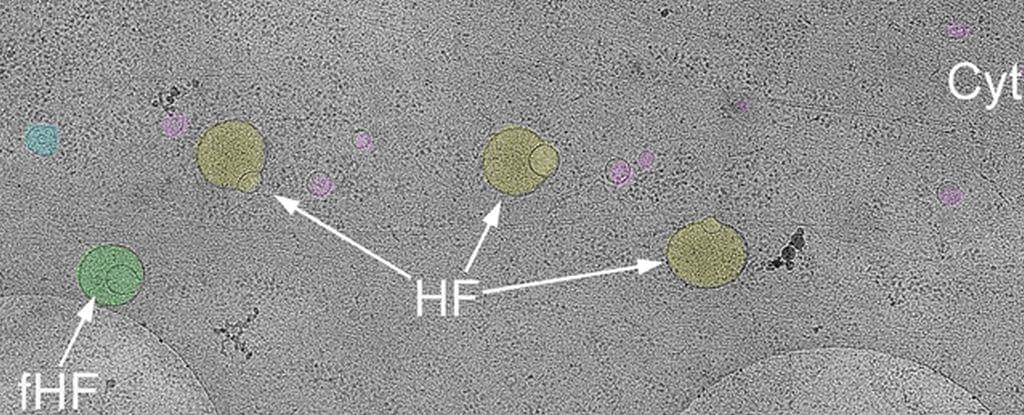
A pioneering new study published in Nature Microbiology, led by J. Oriol Sunyer, professor of immunology and pathobiology at the School of Veterinary Medicine, and a team of researchers at Penn Vet and the University of New Mexico, has uncovered a surprising new player in gut health: an antibody called secretory immunoglobulin M (sIgM).
While another antibody, secretory immunoglobulin A (sIgA), has long been known for helping balance the bacteria in our intestines, this new research shows that sIgM may be just as vital—if not more so—in protecting gut health and maintaining overall well-being.
Secretory immunoglobulins—immunoglobulins found in the mucosal surfaces or linings of various organs and tracts of vertebrates—modulate the colonization, composition, and metabolism of the gut microbiome. While sIgA and secretory immunoglobulin T (sIgT) are considered the key immunoglobulins involved in the maintenance of microbiome homeostasis in the gut of mammals and fish, respectively, Sunyer and his colleagues challenged this paradigm by demonstrating that sIgM plays a crucial and non-redundant role in the regulation of gut microbiota and metabolism.