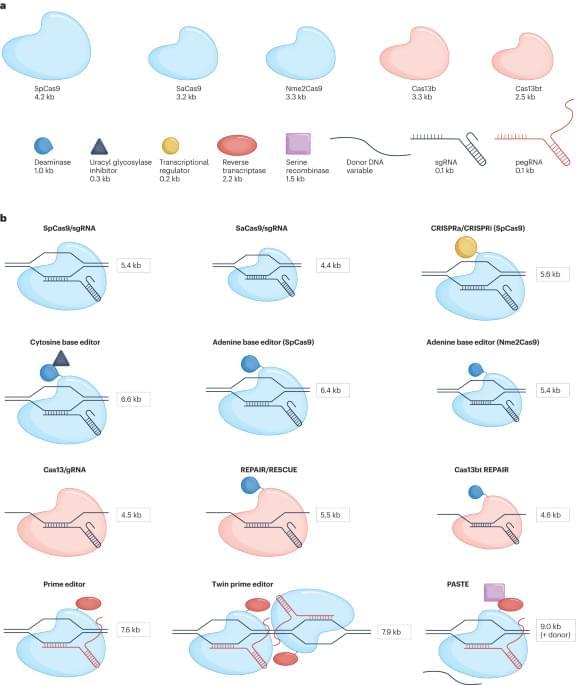
DeepMind has released a catalog of 71 million possible variants that can cause diseases.
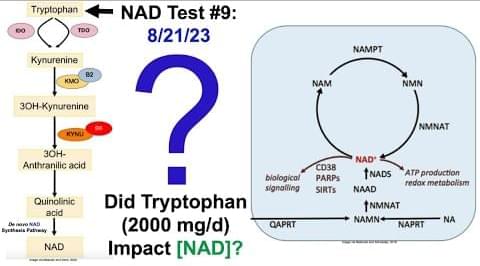
Genetic mutations are changes to our DNA sequence. This happens when cells make copies of themselves during cell division. Mutation is the ultimate source of human genetic variation and has evolutionary and disease genetics implications. A mutation affecting our genes might give birth to a genetic disorder. But just because you have a mutation doesn’t mean it will be a genetic disorder.
That is why researchers at DeepMind, the artificial intelligence arm of Google, have announced that they have trained a machine learning model called AlphaMissense to classify which DNA variations in our genomes are likely to cause disease.