Eliminating old, dysfunctional cells in human fat also alleviates signs of diabetes, researchers from UConn Health report. The discovery could lead to new treatments for Type 2 diabetes and other metabolic diseases.
The cells in your body are constantly renewing themselves, with older cells aging and dying as new ones are being born. But sometimes that process goes awry. Occasionally damaged cells linger. Called senescent cells, they hang around, acting as a bad influence on other cells nearby. Their bad influence changes how the neighboring cells handle sugars or proteins and so causes metabolic problems.
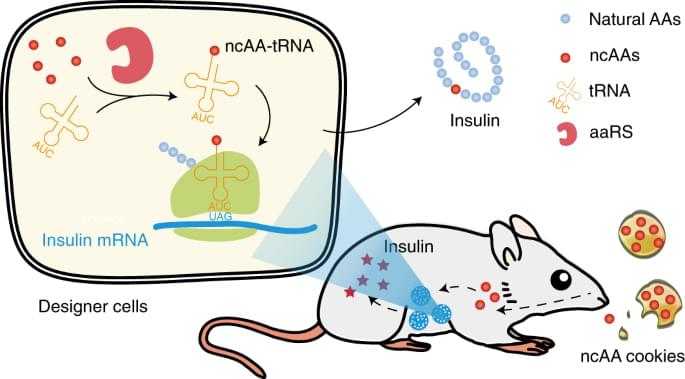
Type 2 diabetes is the most common metabolic disease in the US. About 34 million people, or one out of every 10 inhabitants of the US, suffers from it, according to the Centers for Disease Control and Prevention (CDC). Most people with diabetes have insulin resistance, which is associated with obesity, lack of exercise and poor diet. But it also has a lot to do with senescent cells in people’s body fat, according to new findings by UConn Health School of Medicine’s Ming Xu and colleagues. And clearing away those senescent cells seems to stop diabetic behavior in obese mice, they report in the 22 November issue of Cell Metabolism. Ming Xu, assistant professor in the UConn Center on Aging and the department of Genetics and Genome Sciences at UConn Health, led the research, along with UConn Health researchers Lichao Wang and Binsheng Wang as major contributors. Alleviating the negative effects of fat on metabolism was a dramatic result, the researchers said.