New research reveals that each person has a unique breathing “fingerprint” that can be used to identify them with nearly 97% accuracy.





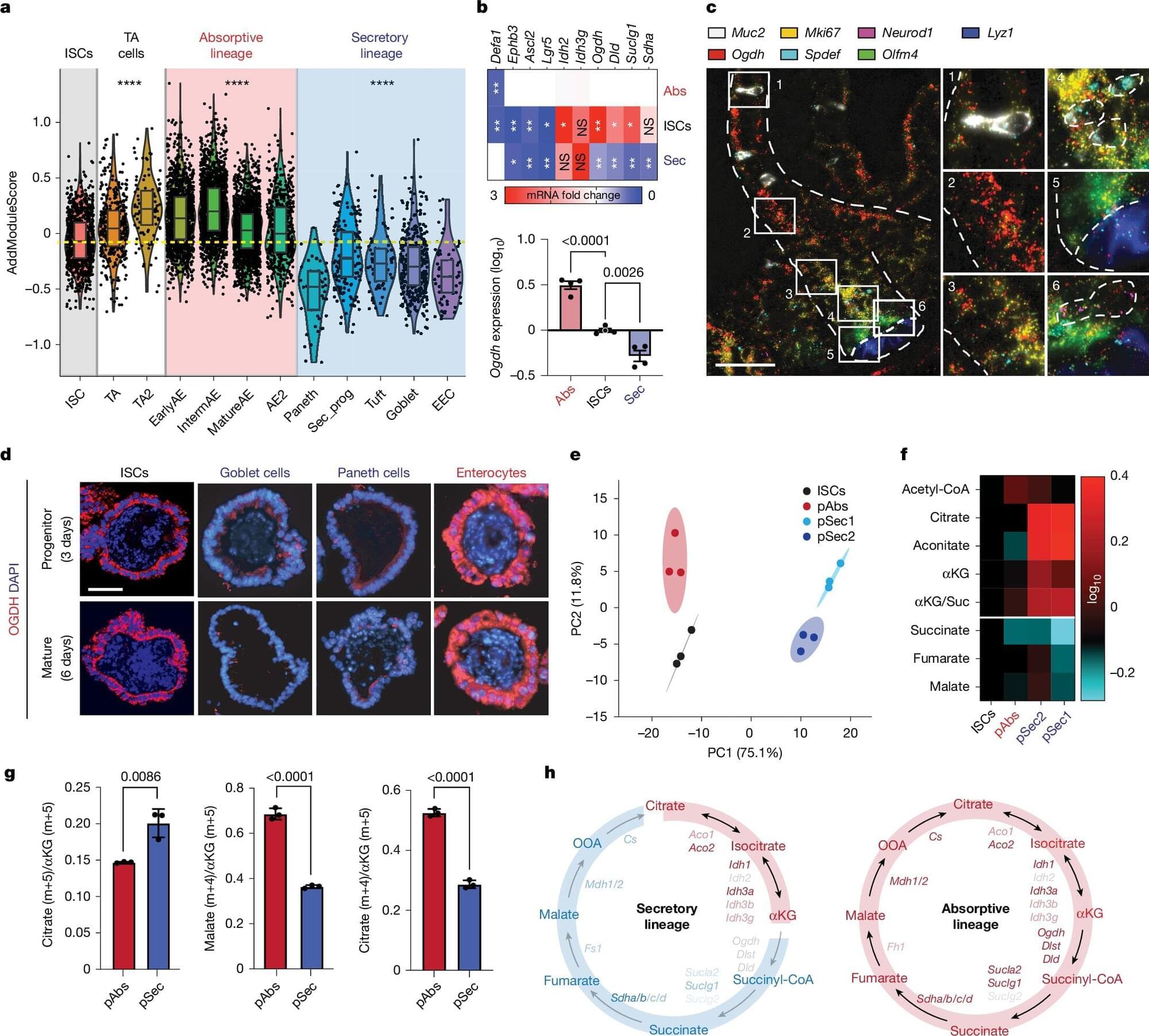
Memorial Sloan Kettering Cancer Center researchers have identified a metabolic switch that determines whether intestinal stem cells become absorptive or secretory cells. Manipulating the enzyme OGDH either fuels cell expansion or redirects fate, with potential consequences for colitis recovery and regenerative therapy.
Stem cells in the intestine maintain a delicate balance between self-renewal and differentiation, continuously replenishing the epithelial lining of the gut.
As they divide, some daughter cells become absorptive enterocytes that expand the surface for nutrient uptake, while others branch into secretory cells that manufacture mucus, antimicrobial peptides, and hormones essential for gut immunity. Injury and inflammation can tip this balance, depleting secretory lineages and disrupting tissue integrity.
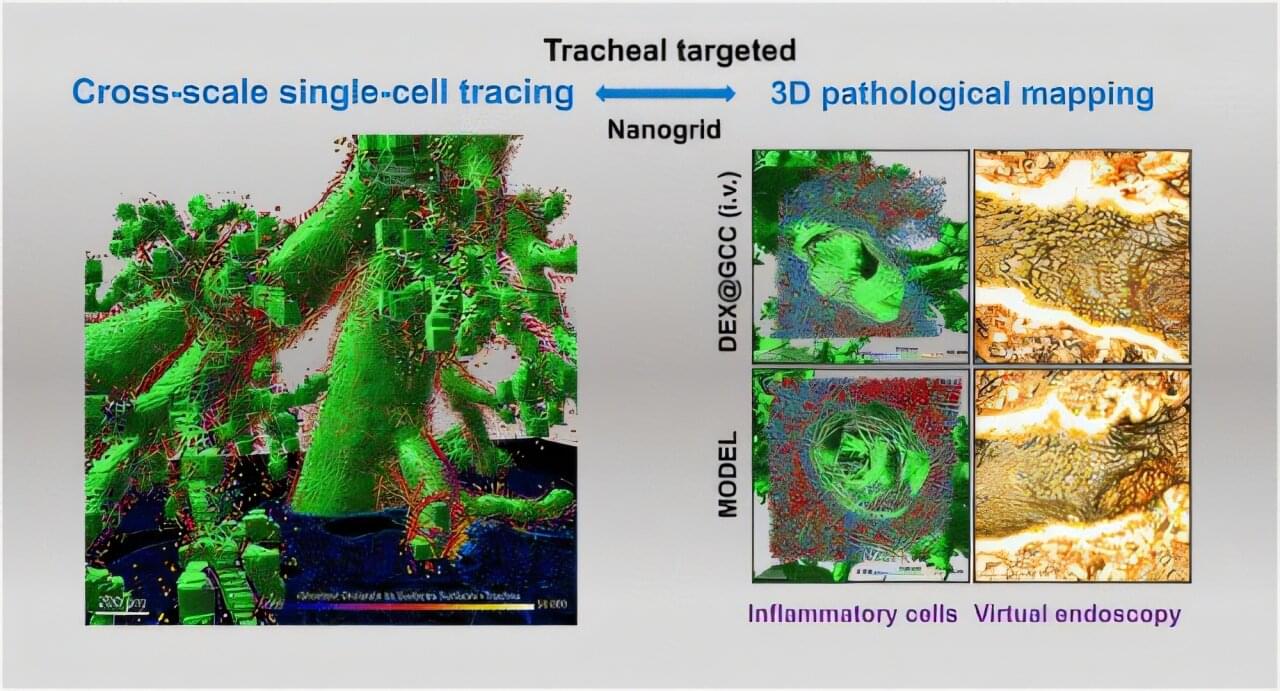
Understanding how drug delivery systems distribute in vivo remains a major challenge in developing nanomedicines. Especially in the lung, the complex and dynamic microenvironment often limits the effectiveness of existing approaches.
“Structural pharmaceutics” has been introduced as a new strategy to connect nanoparticle structures with physiological structures through advanced three-dimensional (3D) imaging and cross-scale characterizations.
In a study published in ACS Nano, a team led by Yin Xianzhen from the Lingang Laboratory and Zhang Jiwen from the Shanghai Institute of Materia Medica of the Chinese Academy of Sciences developed a precise targeting strategy for tracheal inflammation.